CRISPR gene editing represents a revolutionary leap in biotechnology, enabling scientists to modify genetic material with unprecedented precision. This powerful technology holds the potential to eradicate genetic diseases, such as sickle cell anemia, leading to significant advancements in gene therapy. However, the promise of CRISPR comes bundled with a host of ethical concerns that challenge our understanding of health equity and individual rights. As we navigate the complexities of CRISPR technology, it becomes crucial to consider the moral implications of gene manipulation, particularly regarding who gets to decide which traits are deemed desirable. Understanding the risks and responsibilities associated with CRISPR can foster informed discussions about its role in modern medicine and society.
Gene editing technology, particularly the CRISPR system, is at the forefront of discussions around modern genetics and therapeutic innovation. This groundbreaking method allows for the precise alteration of DNA sequences, opening doors for treating hereditary disorders and potentially enhancing human health. Yet, this wave of scientific progress raises significant ethical dilemmas, especially surrounding the notion of genetic equity in healthcare and the societal implications of altering human traits. The conversation includes varying perspectives on responsibilities, from healthcare providers to patients, in the realm of gene therapy and its application in curing conditions like sickle cell disease. As we delve deeper into the landscape of genetic modification, it’s imperative to weigh the benefits against the risks and consider the broader impact on our understanding of health and individuality.
Ethical Concerns Surrounding CRISPR Gene Editing
The advent of CRISPR gene editing technology promises revolutionary treatments for genetic disorders, yet it raises profound ethical concerns. At the forefront of these discussions is the question of whether we should alter human genetics. Does enhancing human traits through gene editing risk undermining the value we place on diversity? Experts in bioethics, like Neal Baer and Rebecca Weintraub Brendel, assert that while the ability to cure diseases like sickle cell anemia is a remarkable achievement, it opens a Pandora’s box of ethical dilemmas. Decisions around which traits to enhance or eliminate could fall into dangerous territory, effectively creating a society that values certain attributes over others, thus risking discrimination rather than fostering inclusion.
Moreover, the actionable insights derived from CRISPR technology necessitate a carefully considered ethical framework. The technology not only enables the possibility of eradicating diseases but also allows modifications that could affect future generations. This initiates a debate on who holds the power to make such critical decisions. Should it be scientists, parents, or governing bodies? These discussions emphasize the need for comprehensive guidelines to navigate the ethical landscape of CRISPR gene editing to avoid misuse and ensure equitable access across diverse populations.
Additionally, the ethics of gene editing extend beyond individual decision-making to broader societal implications, particularly in relation to health equity. As technology advances, there is a risk of creating a divide between those who can afford cutting-edge treatments and those who cannot. The $2.2 million cost associated with the sickle cell gene-editing cure underscores this issue. Without ethical oversight, CRISPR could worsen existing disparities in healthcare access. Ethical discussions become critical when addressing who benefits from such tech advancements, emphasizing that innovation cannot occur in a vacuum devoid of ethics and social responsibility.
Risks Involved in CRISPR Technology
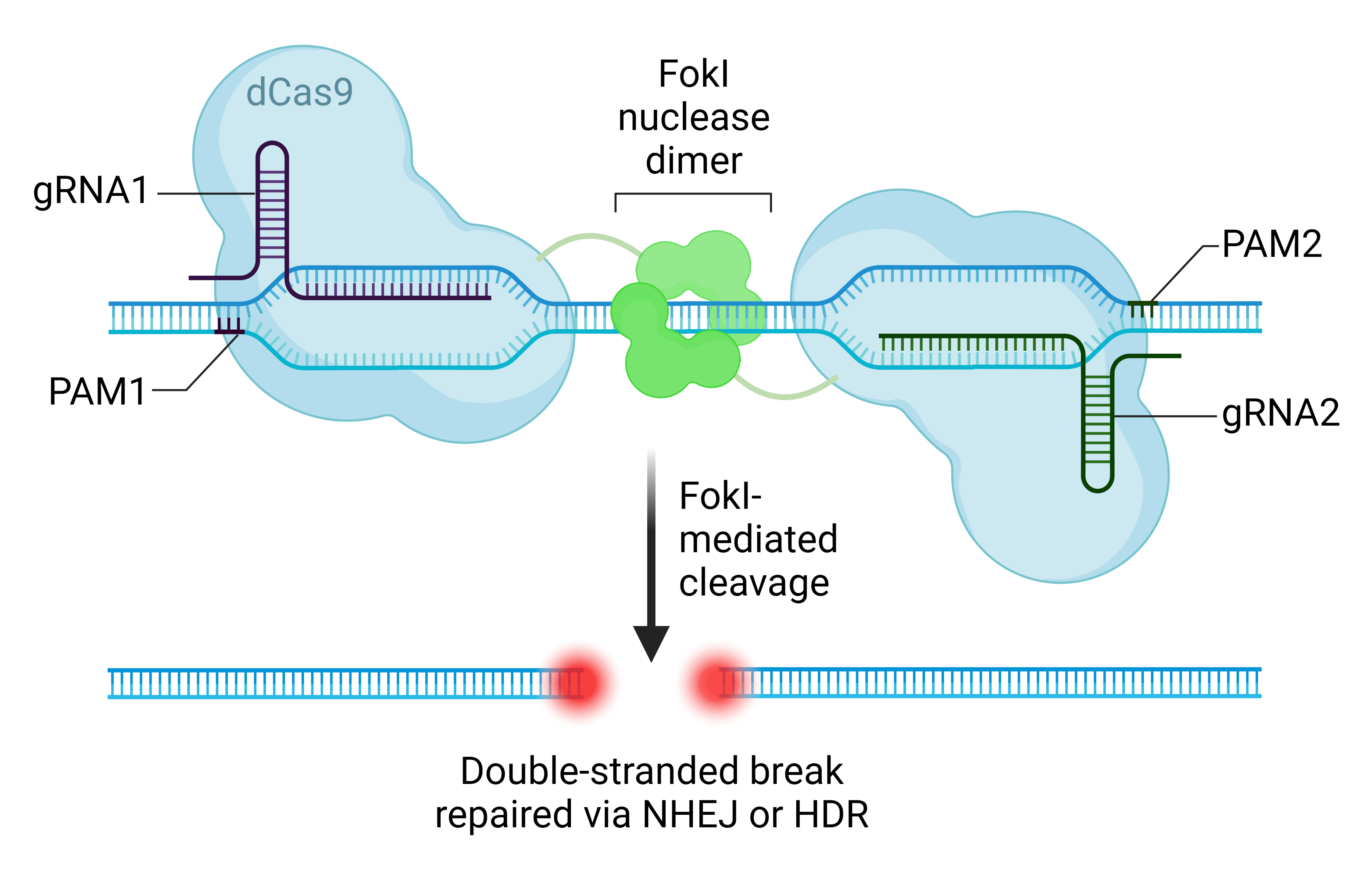
While CRISPR gene editing holds the potential for groundbreaking medical breakthroughs, it is fraught with risks that warrant thorough investigation. One immediate concern is the possibility of unintended consequences arising from genetic modifications. For instance, when altering a gene responsible for a specific condition like high LDL cholesterol, researchers must consider the gene’s interactions with other biological systems. Genetic alterations that aim to provide immediate benefits might inadvertently disrupt essential processes, leading to unforeseen health issues later on, as highlighted by Neal Baer’s discussion on the multifaceted roles genes play in human physiology. These risks call for rigorous studies and long-term monitoring of effects.
Moreover, the rapidly evolving CRISPR technology landscape outruns the current regulatory frameworks designed to handle genetic modifications. The potential for gene editing to be employed without oversight raises critical safety concerns. For instance, the thought of unmonitored gene editing experiments in some countries touches on ethical violations and highlights the need for global regulatory standards. These standards would ensure that gene editing practices are safe, monitored, and used responsibly. Thus, while CRISPR technology provides incredible opportunities for healing, it equally poses significant risks that need to be addressed to safeguard human health and integrity.
Gene Therapy for Sickle Cell Disease: Hope or Hazard?
Gene therapy offers a beacon of hope for individuals suffering from sickle cell disease, and CRISPR technology is leading this charge. By directly editing genes to remove the anomaly that causes this painful condition, CRISPR holds the promise of not just alleviating symptoms but potentially curing the disease entirely. However, with great promise comes great responsibility. The procedural intricacies of implementing such treatments must be handled with precision, considering the long-term implications on health not just for the treated individuals but also for future generations.
The path from experimentation to real-world application requires careful calibration of scientific advancements and ethical considerations. Clinicians and researchers must remain vigilant about the high costs and accessibility of therapies, posing questions not only of feasibility but also of fairness in health solutions. The disparity between available treatments and the ability for diverse populations to access them could exacerbate existing inequities in healthcare, requiring a commitment to ensuring that innovative treatments are accessible and beneficial for all communities.
Furthermore, as scientists explore gene therapy options for sickle cell disease, the broader implications of successful CRISPR applications need consideration. Engaging with communities affected by sickle cell disease is essential for transparent, informed decision-making. These discussions should involve patients and their families to ensure that their values, needs, and aspirations shape the direction of treatment options. It’s crucial that as patients gain access to these therapies, the conversations around patient autonomy and consent are prioritized, thus fostering an environment of trust and respect in medical advancements.
Health Equity in the Era of Gene Editing
The implementation of CRISPR technology brings forth significant advancements in the field of medicine, but it also raises pressing issues of health equity. As treatments become available, disparities in access to cutting-edge technologies may widen the gap between affluent and underprivileged communities. Conversations around health equity must focus on ensuring that all individuals, regardless of their socioeconomic status, have equitable access to gene editing therapies. The disparity in economic capacity could lead to an elite class benefitting from advanced treatments while marginalized groups are left behind, further entrenching health inequities.
Broader societal engagement is crucial in addressing these issues. Stakeholders, including policymakers, must collaborate with medical professionals and communities to develop systems that distribute these transformative technologies fairly. Attention must be paid to the ethical implications of who receives access first and how much each treatment will cost. Health equity should be a driving force in the legislation surrounding gene editing to prevent creating a ‘genetic divide’ that prioritizes profit over patient welfare.
In exploring health equity in gene editing, it is essential to consider the cultural contexts of communities affected by genetic disorders. Engaging with diverse populations in dialogue surrounding gene therapy can help ensure that local values and ethical considerations shape the rollout of CRISPR treatments. This approach fosters trust between medical practitioners and community members, ensuring that public health initiatives are not only effective but also respectful and representative of the communities they aim to help. Educating these communities about CRISPR technology, its benefits, and its risks will empower individuals to make informed decisions about their health, leading to a more equitable healthcare landscape.
Doctor’s Ethical Implications of Gene Editing
For medical professionals, the rise of CRISPR technology introduces complex ethical dilemmas that significantly impact their responsibilities toward patients. Doctors must navigate the delicate balance between advancing healthcare through innovative treatments and upholding ethical standards that prioritize patient welfare. The ethical implications of gene editing extend to making informed decisions that align with the best interests of the patient while considering long-term societal impacts. Such weighty considerations invite a reevaluation of what it means to practice medicine in the age of genetic editing, prompting many practitioners to reflect on their roles as both healers and ethical stewards in a rapidly evolving landscape.
Additionally, the evolving nature of CRISPR technology calls for continuous education and discussion among healthcare providers regarding the ethical, legal, and social implications of gene editing. Medical professionals must prepare to address questions surrounding not only clinical efficacy but also the moral complexities that accompany each decision regarding genetic interventions. This ongoing dialogue is critical to remain accountable and to instill confidence among patients, ensuring that the practice of gene editing is guided by ethical principles centered around non-maleficence, beneficence, and justice.
Furthermore, the potential repercussions of CRISPR technology compel doctors to consider the societal implications of their decisions. The ethical responsibility of practitioners extends beyond individual cases, raising questions about the collective impact of gene editing on society as a whole. For instance, creating genetically modified offspring to fulfill parental desires raises ethical issues about consent and the rights of future generations. Thus, the doctor’s role evolves into one that must continuously reassess the moral frameworks guiding their practice, advocating for informed dialogues about CRISPR technology not only within clinical settings but also within public health conversations. It is fundamental that the medical community leads these discussions, fostering informed consent and ethical awareness among patients and their families.
Frequently Asked Questions
What are the ethical concerns surrounding CRISPR gene editing?
The ethical concerns surrounding CRISPR gene editing include the potential for making significant changes to human genetics that could lead to unforeseen consequences, such as affecting not just health but also traits considered non-pathological, like intelligence or physical abilities. There is a fear of exacerbating health inequities, as access to this technology may be limited to wealthier populations, and questions arise about who should have the authority to decide which genes are modified.
How does CRISPR technology impact gene therapy for sickle cell disease?
CRISPR technology offers a revolutionary approach to gene therapy for sickle cell disease by allowing scientists to directly edit the genes responsible for the disorder. This can lead to effective treatments that remove the disease-causing genes from patients’ somatic cells, potentially curing them and improving their quality of life. However, ethical implications around access and the cost of such treatments need to be carefully considered.
What are the risks associated with CRISPR technology?
The risks associated with CRISPR technology include unintended genetic alterations, which may lead to unforeseen health issues or genetic disorders. Furthermore, the long-term effects of editing germline cells remain largely unknown, raising concerns about the potential hereditary impacts on future generations. There is also the concern that CRISPR could be misused for enhancements rather than therapeutic purposes, leading to ethical dilemmas.
How does health equity relate to CRISPR gene editing?
Health equity is a critical issue in the context of CRISPR gene editing, as the high costs associated with gene editing treatments, like those for sickle cell disease, may limit access for underprivileged populations. This could result in a wider gap in healthcare quality and outcomes between different socioeconomic groups, leading to ethical discussions about fairness, accessibility, and how to ensure that all communities benefit equally from advancements in CRISPR technology.
What are the ethical implications of CRISPR gene editing as discussed by medical professionals?
Medical professionals emphasize the ethical implications of CRISPR gene editing, highlighting the need for oversight and responsible use. This includes evaluating the moral responsibilities of parents in choosing genetic attributes for their children, the potential for misuse of gene editing for non-medical enhancements, and ensuring that decisions about gene modification take into account broader social and ethical contexts to avoid exacerbating inequalities.
| Key Points | Details |
|---|---|
| Ethical Dilemma | The discussion highlights whether we should modify human traits or conditions. |
| Life-Altering Potential of CRISPR | CRISPR can cure conditions like sickle cell anemia but raises questions about who decides the merit of such changes. |
| Financial Concerns | The cure for sickle cell anemia costs around $2.2 million, raising issues of affordability and access. |
| Health Justice | Innovations like gene editing may widen existing health inequities. |
| Parental Rights | Debate exists over whether parents should make genetic decisions for their children. |
| Oversight Issues | There are concerns about monitoring gene editing practices globally, particularly in countries without strict regulations. |
| Unintended Effects | Gene editing may have unforeseen consequences due to complex gene interactions. |
Summary
CRISPR gene editing represents a groundbreaking advancement in genetics with the potential to cure serious disorders like sickle cell anemia. However, it brings forth a myriad of ethical dilemmas concerning human modification, equity in healthcare access, and the responsibilities of scientific innovation. As we navigate these uncharted waters, it is crucial to maintain a robust dialogue about the moral implications of such technologies, ensuring that progress does not come at the expense of societal values.