Pediatric cancer recurrence remains one of the most pressing challenges in the medical field, particularly for families affected by conditions like gliomas. Recent advancements in AI could significantly change the landscape of cancer risk prediction, allowing for more accurate assessments of brain tumor recurrence among young patients. In a groundbreaking study, researchers leveraged cutting-edge technology to analyze multiple brain scans over time, dramatically improving predictions of relapse compared to traditional methods. This innovative approach not only enhances our understanding of pediatric gliomas but also offers hope for better individualized treatment plans and outcomes. As we continue to explore the intersection of AI in pediatric cancer care, it is vital to prioritize early detection and tailored therapies to combat the emotional and physical toll of recurrence.
The recurrence of childhood cancer is a critical concern for many families, particularly when it involves aggressive forms of tumors such as brain cancers or gliomas. Advances in predictive analytics, especially through the use of artificial intelligence, are paving the way for improved assessments of relapse risks for young patients. By utilizing comprehensive imaging techniques, healthcare professionals can gain insights into the likelihood of brain tumor recurrence, ultimately leading to better-informed treatment decisions. Understanding the dynamics of pediatric cancers and their potential return is crucial for designing effective therapeutic strategies. As research progresses, the incorporation of sophisticated AI models may transform how we approach long-term monitoring and care for children battling these serious conditions.
Understanding Pediatric Cancer Recurrence
Pediatric cancer recurrence is a critical concern for healthcare providers and families alike. Many young patients diagnosed with conditions like gliomas, a type of brain tumor, often face the fear of the cancer returning after treatment. Unlike adult cancers, which can exhibit more predictable behavior, pediatric cancers can vary greatly in their recurrence patterns. This unpredictability necessitates ongoing monitoring and innovative approaches to patient care, which is where new technology, particularly artificial intelligence, is making significant inroads.
The application of AI in predicting the likelihood of pediatric cancer recurrence marks a transformational change in the approach to managing these cases. Traditional methods have relied heavily on individual imaging studies and patient histories, which can be limiting and inaccurate. Now, advanced AI algorithms can analyze multiple brain scans over time, identifying subtle changes that may indicate a risk of recurrence far better than any human could. By effectively harnessing large datasets, AI provides insight that empowers clinicians to make more informed decisions regarding follow-ups and treatments.
The Role of AI in Pediatric Cancer Management
AI technologies, particularly those designed for analyzing medical imaging, play an increasingly pivotal role in the management of pediatric cancers like gliomas. These advanced systems utilize a process known as temporal learning, allowing them to consider a sequence of scans over time rather than judging from a singular image. This method has proven to enhance prediction accuracy significantly, shifting the paradigm from traditional predictive methods to a more dynamic, comprehensive view of patient health.
Moreover, the implementation of AI-driven decision-making tools does not just assist in predicting brain tumor recurrence; it has the potential to reshape the overall treatment landscape for young patients. For instance, knowing precisely when and how a cancer might recur can lead to personalized patient care, minimizing the burden of unnecessary procedures for low-risk patients while ensuring high-risk patients receive timely, targeted therapies. This tailored approach could significantly improve outcomes and quality of life for pediatric patients battling cancer.
Enhancing Diagnosis with AI in Pediatric Gliomas
Pediatric gliomas present unique challenges due to their diverse nature and varying responses to treatment. With new AI tools emerging, the potential to enhance diagnostic accuracy and predict relapse is starting to become a reality. Researchers have demonstrated that by leveraging large datasets of MR scans, AI can identify patterns that may indicate the presence of disease progression or recurrence, thus allowing for earlier intervention and improved patient outcomes.
Additionally, integrating AI into clinical workflows helps to streamline the process of monitoring pediatric gliomas. As families often face considerable emotional and financial stress during the treatment journey, AI can potentially reduce the frequency of rigorous imaging for patients classified as low-risk, based on AI predictions. This not only alleviates anxiety for families but also allows healthcare professionals to allocate resources more efficiently, focusing their efforts on those patients with a higher likelihood of recurrence.
Breakthroughs in Cancer Risk Prediction Using AI
Recent advancements in AI technology have spotlighted its ability to redefine cancer risk prediction across pediatric oncology. By analyzing thousands of imaging studies, researchers have developed sophisticated algorithms capable of identifying nuanced changes in brain scans that are indicative of potential glioma recurrence. This predictive capability offers a beacon of hope for enhancing survival rates by enabling timely interventions that were previously considered too uncertain.
The implications of improved cancer risk prediction extend beyond individual clinics. With ongoing research leading to higher accuracy in recurrence predictions, there is the potential for these AI solutions to be integrated into broader healthcare systems, effectively transforming pediatric cancer management on a national and possibly global scale. The ability to predict cancer risks tailored to the individual patient could revolutionize pediatric healthcare, ensuring that every child receives the most appropriate care based on their specific risk profile.
Innovative Techniques: Temporal Learning in AI
The introduction of temporal learning in the context of AI modeling represents a significant advancement in medical imaging. Unlike traditional models that analyze a single MR scan at a time, temporal learning utilizes a series of scans taken at various time points. This comprehensive analysis not only improves accuracy in predicting pediatric cancer recurrence but also offers insights into the fluctuations in tumor behavior following initial treatment.
By recognizing patterns across multiple imaging sessions, AI can inform clinicians about the likelihood of glioma recurrence in pediatric patients more effectively than before. This innovation holds great promise for practice, enabling healthcare providers to shift from reactive to proactive treatment strategies, thus optimizing care pathways for children and reducing the long-term impacts of cancer treatment.
The Future of Pediatric Cancer Treatment
The future of pediatric cancer treatment is increasingly being shaped by technological advancements, particularly through AI and machine learning. As research continues to validate the effectiveness of these tools, their integration into clinical practice promises to improve not only the accuracy of diagnoses but also the timing of interventions. With studies showing improved predictions of glioma recurrence rates, healthcare providers can tailor surveillance strategies and treatment plans more effectively.
As AI further evolves in the context of pediatric cancers, the goal will be to refine its applications to enhance patient outcomes continuously. By mapping the journey of cancer treatment and recurrences, healthcare professionals can ensure that care is as individualized as possible, depending upon the unique dynamics of each patient’s illness. This personalized approach can ultimately lead to more successful interventions and improved quality of life for young patients confronting the challenges of childhood cancer.
Challenges in Implementing AI in Pediatric Oncology
Despite the remarkable potential AI holds for pediatric oncology, several challenges lie ahead in its implementation. One of the primary concerns involves the validation of AI models across diverse patient populations and clinical settings. For AI predictions to be generalizable, large-scale trials must demonstrate that the findings can be applied in varying contexts, ensuring that all pediatric patients benefit from these advancements regardless of their location or background.
Additionally, integrating AI technology with existing healthcare systems poses its challenges, including the need for adequate training for medical professionals. While AI provides sophisticated tools for predicting pediatric cancer recurrence, physicians must be well-equipped to interpret these results accurately and make informed decisions based on AI recommendations. Addressing these issues will be crucial to unlocking the full potential of AI in transforming treatment paradigms within pediatric oncology.
The Impact of AI on Family Experiences
The journey of a child battling cancer is undeniably stressful and filled with uncertainties for families. The advent of AI and its applications in predicting pediatric cancer recurrence aims to alleviate some of these burdens. By providing more accurate forecasts regarding the likelihood of a relapse, families can make more informed decisions regarding their child’s care and create a more structured approach to treatment plans.
Furthermore, with AI tools reducing the frequency of imaging for low-risk patients and potentially allowing for less intrusive monitoring methods, families can experience a sense of relief from the constant fear of what lies ahead. The emotional weight that comes with frequent MR scans can be daunting; however, by leveraging AI’s predictive capabilities, families may find solace in knowing their child’s condition is being closely monitored by advanced technologies designed to protect and promote their health.
Closing Thoughts on AI in Pediatric Oncology
As we continue to embrace AI’s potential in pediatric oncology, the collaborative efforts of researchers, clinicians, and technology developers become increasingly essential. Ongoing studies and initiatives aimed at enhancing AI applications will provide critical insights that can lead to significant advancements in how we understand and treat pediatric cancers, particularly when it comes to predicting outcomes related to glioma recurrence.
Ultimately, the goal is to establish a care model that prioritizes the unique needs of pediatric patients while minimizing stressors and maximizing health outcomes. By focusing on integrating advanced technology like AI into standard practices, the future of pediatric cancer care looks promising, offering hope and improved quality of life for families navigating the challenging landscape of childhood cancer.
Frequently Asked Questions
What is pediatric cancer recurrence and how is it related to glioma treatment?
Pediatric cancer recurrence refers to the return of cancer in children after treatment, particularly in cases like pediatric gliomas, which are brain tumors that can arise in young patients. Treatment typically includes surgery, but understanding the risk of recurrence is crucial for ongoing management. Advanced techniques, such as AI in pediatric cancer care, are being developed to better predict these instances of recurrence, helping to tailor follow-ups and interventions.
How does artificial intelligence improve cancer risk prediction in pediatric gliomas?
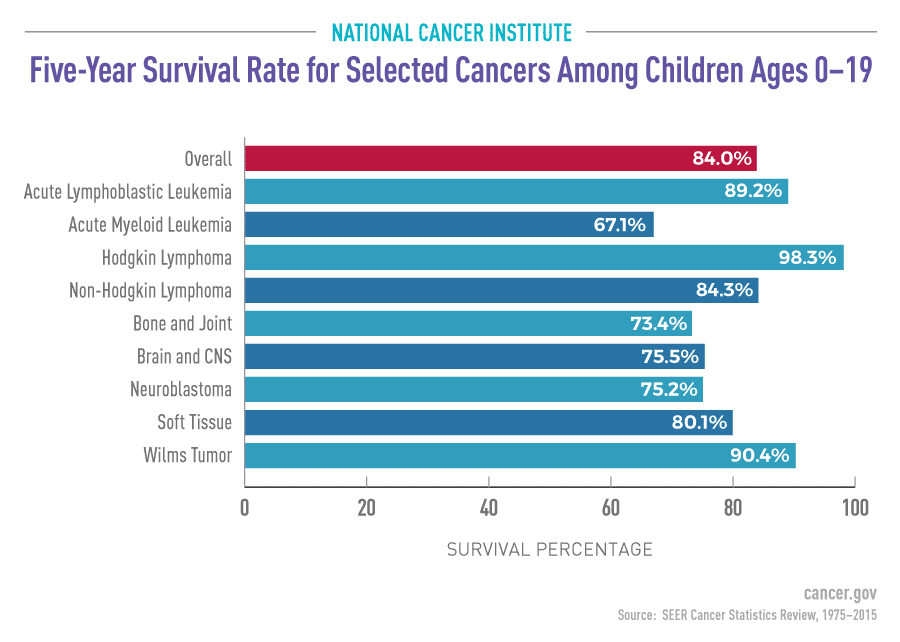
Artificial intelligence enhances cancer risk prediction in pediatric gliomas by analyzing longitudinal imaging data, allowing for improved identification of patients at risk for tumor recurrence. Traditional methods often rely on single MR images, while AI employs temporal learning, which considers multiple scans over time, increasing prediction accuracy to 75-89% for recurrence.
What role does AI play in predicting brain tumor recurrence in pediatric patients?
AI plays a transformative role in predicting brain tumor recurrence in pediatric patients by utilizing advanced algorithms to assess multiple MRI scans over time. This innovative approach enhances the understanding of tumor behavior post-surgery, providing healthcare providers with better tools to detect high-risk patients early and adjust treatment protocols accordingly.
What findings were revealed in the study regarding pediatric glioma recurrence?
The study found that using an AI model trained with temporal learning significantly improved predictions of pediatric glioma recurrence. It achieved accuracy rates between 75-89%, which greatly surpasses traditional methods that predict recurrence using a single scan at about 50% accuracy. These findings emphasize the potential of AI tools in enhancing clinical outcomes for children with brain tumors.
How does temporal learning affect predictions of pediatric cancer recurrence?
Temporal learning improves predictions of pediatric cancer recurrence by allowing AI models to analyze a series of MRI scans taken over time rather than isolated images. This method helps identify subtle changes in tumor characteristics, which are crucial in predicting whether a pediatric glioma might recur, ultimately leading to more informed treatment decisions.
What are the implications of improved cancer risk prediction for pediatric glioma patients?
Improved cancer risk prediction for pediatric glioma patients means better management strategies, such as reducing unnecessary imaging for low-risk patients or initiating early treatment for those at high risk of recurrence. This personalized approach not only alleviates the emotional and financial burden on families but may also enhance the overall outcomes in pediatric oncology.
What challenges remain in the application of AI for predicting pediatric cancer recurrence?
Despite promising findings, challenges in applying AI for predicting pediatric cancer recurrence include the need for further validation across diverse clinical settings and ensuring the reliability of AI tools in routine practice. Ongoing clinical trials are needed to confirm these predictive models can effectively improve patient care and outcomes.
Why is it important to understand pediatric cancer recurrence risk in children?
Understanding pediatric cancer recurrence risk is essential because it helps healthcare providers tailor surveillance and treatment plans for young patients. Since relapses can be devastating, particularly with pediatric gliomas, accurately predicting which children may be at higher risk allows for timely interventions, improving the chances of successful outcomes.
| Key Point | Detail |
|---|---|
| AI Tool for Prediction | An AI tool provides better predictions of relapse risk in pediatric cancer patients compared to traditional methods. |
| Study Context | The study involved nearly 4,000 MR scans from 715 pediatric patients and aimed to enhance care for those with gliomas. |
| Temporal Learning Technique | Temporal learning trains the AI to analyze multiple brain scans over time, improving accuracy in predicting recurrence. |
| Prediction Accuracy | The model achieved a prediction accuracy of 75-89%, significantly higher than the 50% accuracy from single images. |
| Clinical Application | Researchers hope to initiate clinical trials to validate AI predictions and improve treatment protocols. |
Summary
Pediatric cancer recurrence is a critical concern for healthcare professionals, and recent advancements using AI technology may address this challenge effectively. The new AI tool developed by researchers from Mass General Brigham outperforms traditional methods in predicting relapse risk for pediatric gliomas. By employing temporal learning, the AI analyzes multiple MRI scans taken over time, enhancing prediction accuracy and thereby improving potential treatment outcomes. As studies continue, the hope is that AI will reshape the monitoring protocols for at-risk children, leading to better management of pediatric cancer recurrence.