Infant mortality rates remain a critical issue in the United States, highlighting significant healthcare inequalities between racial groups. Recent studies reveal a troubling disparity: while overall mortality rates have improved for both Black and white Americans, the mortality rate for Black infants is alarmingly higher—now approximately twice that of their white counterparts. This racial disparity in healthcare showcases not only the differences in access to quality care but also the underlying systemic issues that contribute to such inequalities. Factors influencing health outcomes include socioeconomic status, medical care accessibility, and social determinants of health, all of which play crucial roles in the survival of infants. Addressing these inequities is essential for improving life expectancy differences and ensuring that every child, regardless of race, has the opportunity for a healthy start in life.
The topic of neonatal mortality reveals significant disparities in healthcare systems, particularly when examining infant fatalities among different racial groups. While overall health outcomes have shown positive trends over the decades, the stark contrast between Black and white neonatal deaths raises urgent questions about the fairness and effectiveness of current medical practices. Over the years, crucial factors leading to these outcomes, such as access to healthcare, quality of prenatal and neonatal services, and socioeconomic influences, have remained inadequately addressed. This situation emphasizes the importance of recognizing and rectifying inequities within health systems to promote equitable care for all infants. Understanding these patterns will drive essential policies to bridge the gaps that persist in infant health.
The Concerning Rate of Black Infant Mortality
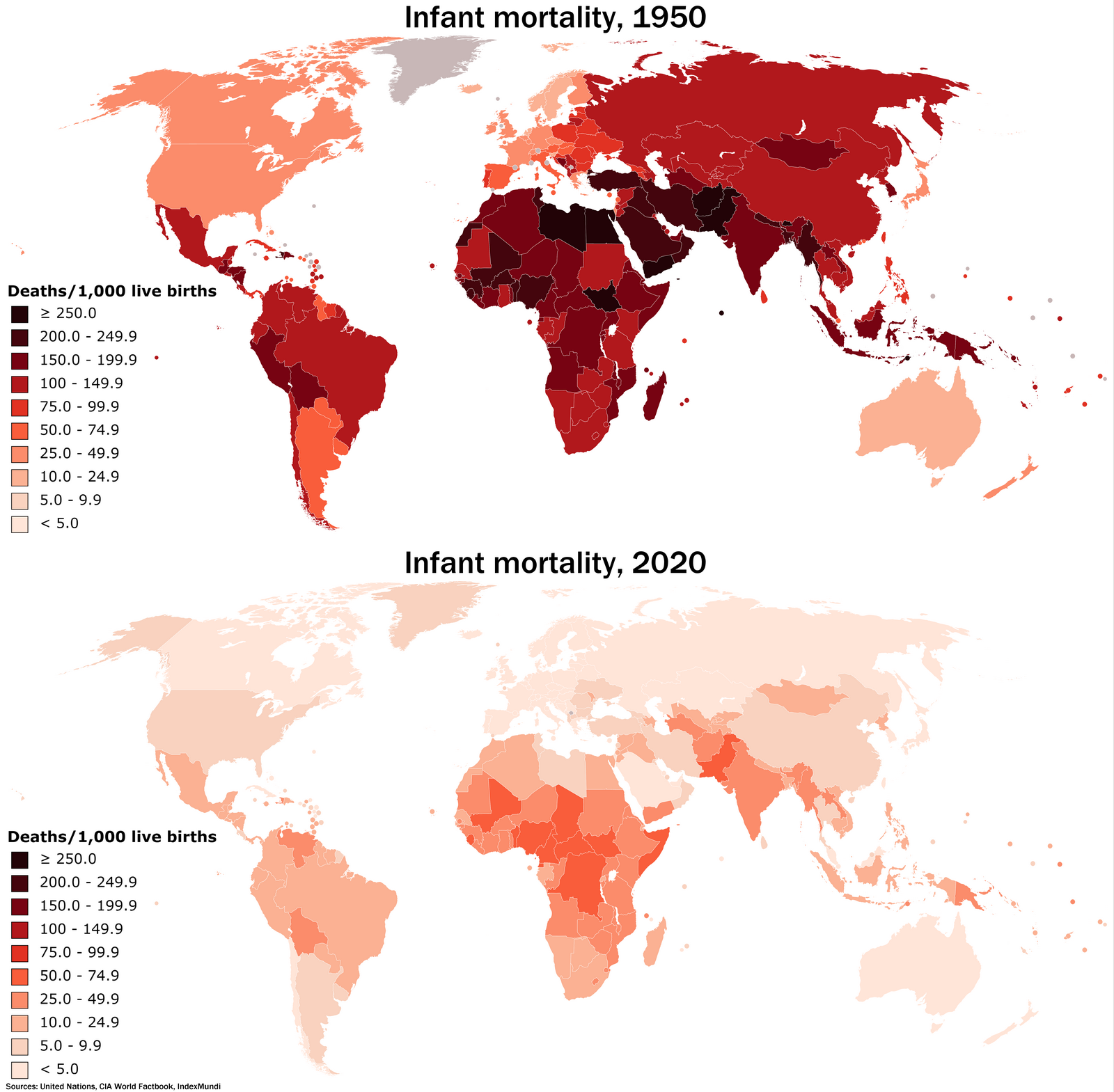
The alarming reality of Black infant mortality rates stands stark against the backdrop of general improvements in life expectancy for both racial groups in the United States. Despite advancements in adult healthcare, the mortality rate for Black infants remains distressingly high—now at twice that of their white counterparts. This discrepancy, which has grown from a 92% higher mortality rate in the 1950s to a staggering 115% today, urges immediate attention from public health officials and policymakers. The nuanced complexities surrounding these numbers signal deep-rooted issues within the healthcare system, specifically pointing towards systemic healthcare inequality and the need for focused intervention.
Such a persistent gap in infant mortality rates underscores the multiple dimensions of healthcare inequality impacting Black communities. Factors such as inadequate access to quality prenatal care and socioeconomic disparities contribute significantly to these outcomes. Medical conditions during pregnancy, which were found to be the primary cause of excess deaths among Black infants in recent years, highlight the critical need for targeting healthcare access and improving maternal health outcomes. To address this racial disparity in healthcare effectively, a multi-faceted approach involving policy reform, community engagement, and educational initiatives is essential.
Racial Disparities and Their Impact on Health Outcomes
Racial disparities in healthcare continue to shape health outcomes across the United States, contributing to significant differences in mortality rates among Black and white populations. While the overall mortality gap has narrowed over the last 70 years, the specific situation for Black infants starkly contrasts this trend. Improvements in healthcare for adults do not necessarily translate to better outcomes for infants, indicating a need for tailored interventions that address both access and quality of care specifically for Black families. This ongoing disparity in healthcare quality perpetuates cycles of disadvantage, affecting future generations and exacerbating life expectancy differences.
The impact of such healthcare inequities extends beyond mere statistics. The lived experiences of families dealing with the grief of losing an infant due to preventable healthcare failures are profound and devastating. Research suggests that over the past 70 years, as many as 5 million Black lives could have been saved if healthcare access and quality were comparable to that of white Americans. This realization serves as a stark reminder that substantial improvement in population health can only be achieved when racial disparities in healthcare are systematically addressed.
Healthcare Inequality: A Call for Policy Reform
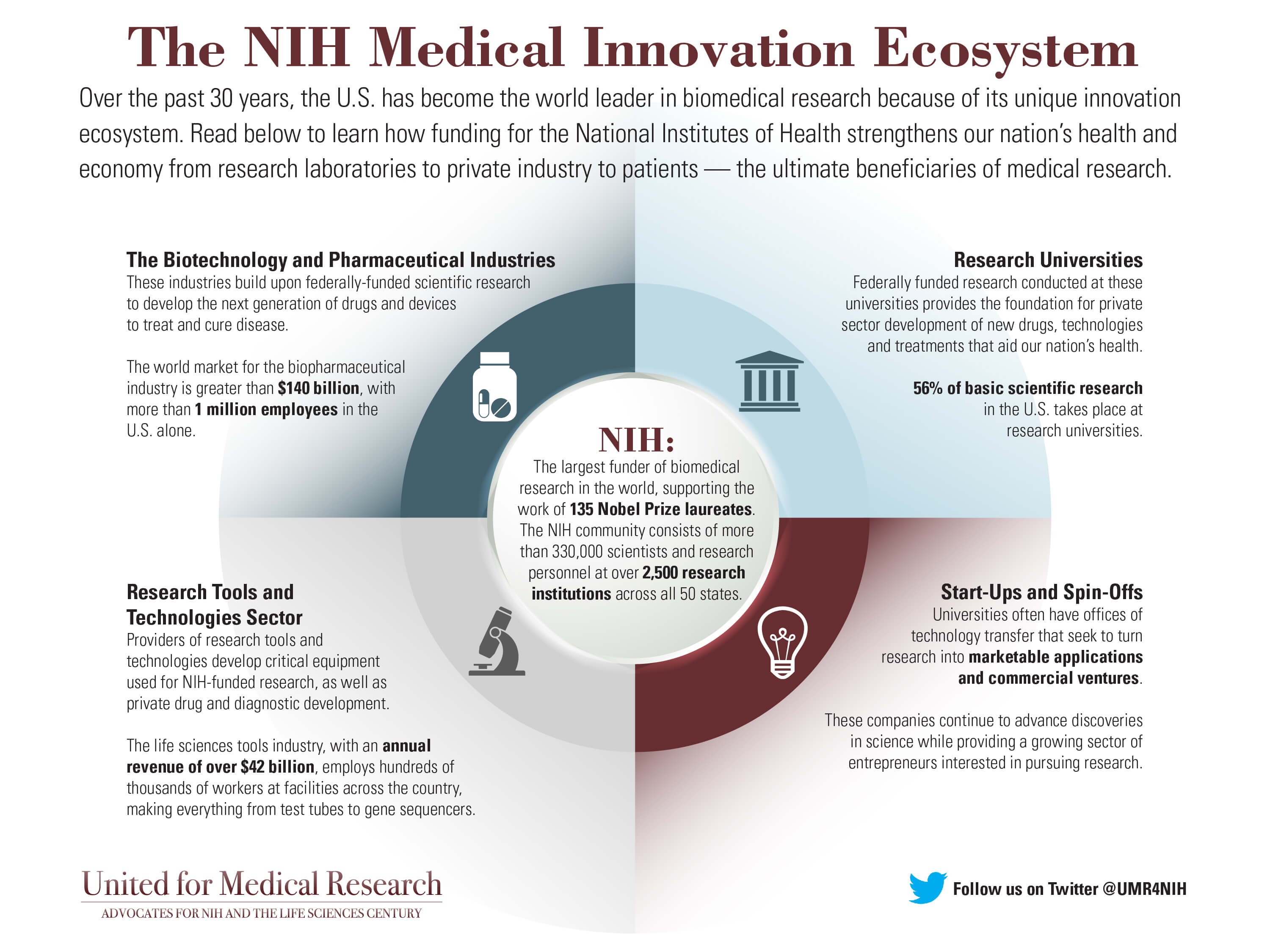
The persistent healthcare inequality affecting Black Americans demands urgent policy reform aimed at eradicating disparities in access and outcomes. Although life expectancy has improved overall, the associated benefits have not been shared equally across racial lines. The findings from recent studies highlight that public health officials must reassess current strategies to ensure equitable healthcare practices that effectively address the unique challenges faced by Black infants and their families. Policymakers should prioritize initiatives that focus on enhancing maternal health support, expanding access to healthcare services, and investing in community-based health programs.
Addressing these critical areas can pave the way for significant improvements in infant mortality rates and overall health outcomes for marginalized populations. Effective policy reforms must integrate social determinants of health, which include socioeconomic status, education, and neighborhood environment, into healthcare planning and delivery. By adopting a comprehensive approach that includes equitable resource distribution and targeted outreach, the healthcare system can begin to dismantle the barriers perpetuating racial disparities, ultimately improving the quality of life for all.
Understanding Life Expectancy Differences Amidst Racial Inequality
Life expectancy differences between racial groups continue to be a crucial measure of public health and social equity. Recent studies indicate that while life expectancy has increased for both Black and white Americans, the gaps in infant mortality rates highlight the disparities that persist. These differences in life expectancy cannot be viewed in isolation, as they are directly influenced by social determinants that shape health outcomes from birth. A focused examination reveals that Black infants are at a higher risk of mortality due to a combination of factors including healthcare access inequalities, socioeconomic challenges, and systemic discrimination in healthcare settings.
Understanding these life expectancy differences requires a robust analysis of the factors contributing to unequal health outcomes. System-wide changes in healthcare delivery must acknowledge the historical injustices faced by Black communities and aim to rectify them. By prioritizing comprehensive healthcare reforms that target these disparities, society can begin to make strides toward not just equal life expectancy but also equitable health outcomes for all infants, regardless of race.
The Role of Public Health Authorities in Addressing Disparities
Public health authorities play a crucial role in addressing and mitigating the disparities that exist in infant mortality rates among different racial groups. Their responsibility extends beyond merely recording statistics; they must actively engage in creating targeted interventions to improve healthcare access and quality for Black infants. This includes advocating for policies that prioritize maternal and infant health, alongside increasing funding and resources for healthcare facilities in underserved communities. Engaging community stakeholders can help ensure that health programs are culturally relevant and effectively meet the needs of the population.
Furthermore, public health initiatives should focus on raising awareness about the ongoing disparities and mobilizing efforts towards community education. By providing mothers with vital information about prenatal care and infant health, authorities can empower families to make informed decisions that positively impact their health outcomes. The synergy between policy reform, community engagement, and public health advocacy is essential for tackling the root causes of racial disparities in healthcare, ultimately leading to improved health outcomes for Black infants.
Potential Solutions to Reduce Black Infant Mortality
Finding solutions to reduce Black infant mortality rates requires a multi-dimensional approach that addresses the various factors contributing to disparities in healthcare. Among the most effective strategies is enhancing access to quality prenatal care for Black mothers, which is crucial in mitigating risks during pregnancy and childbirth. Policy changes that improve healthcare systems, including expanding Medicaid coverage and providing support for maternal health programs, can significantly influence outcomes. Such measures should be paired with community-driven initiatives that prioritize the needs of Black families and focus on culturally competent care.
In addition to improving access, addressing broader social determinants of health is fundamental to reducing infant mortality. Issues such as housing insecurity, education access, and economic stability must be considered in creating effective interventions. Collaborative efforts involving healthcare providers, policymakers, and community leaders are vital to fostering an environment where Black infants have a greater chance of survival. Implementing comprehensive solutions that integrate equitable healthcare access, community support, and policy advocacy can contribute to significant improvements in reducing Black infant mortality rates over time.
The Importance of Longitudinal Studies in Understanding Racial Disparities
Longitudinal studies serve as a critical tool in understanding the dynamics of racial disparities, particularly in healthcare outcomes such as infant mortality rates. The comprehensive nature of these studies allows researchers to track changes over several decades, revealing trends that shorter studies may overlook. The recent analysis of mortality rates from the 1950s to the present demonstrates that while life expectancy for adults has improved, the situation for Black infants has not only stagnated but worsened. Such insights underscore the importance of examining historical data when assessing the effectiveness of healthcare systems and interventions.
Incorporating longitudinal analysis can significantly enhance policymakers’ understanding of the systemic inequalities that persist in healthcare. It allows for informed decision-making that goes beyond surface-level observations, shedding light on the long-term impact of policy choices on different racial groups. By utilizing findings from extensive data collections, health officials can devise strategies that specifically target the root causes of disparities, ultimately leading to improved health outcomes for infants and recognition of the ongoing challenges faced by marginalized communities.
Engaging Communities to Address Healthcare Inequality
Community engagement is essential in the fight against healthcare inequality, particularly regarding infant mortality rates among Black populations. Building trust and fostering relationships with local communities allows healthcare providers and policymakers to better understand the unique challenges they face. Culturally specific outreach programs can help disseminate important health information, encourage access to care, and empower families to advocate for their health needs. By collaborating with community leaders, health organizations can create effective systems of support that resonate with individuals and inspire action towards collective health improvement.
Moreover, amplifying the voices of those directly affected by healthcare disparities creates pathways for meaningful change. Engaging with families to identify barriers to care and develop solutions that reflect their experiences is crucial. This collaborative approach helps ensure that interventions are not only effective but also culturally sensitive, ultimately leading to higher utilization of healthcare resources. As communities continue to navigate systemic inequalities, prioritizing engagement and collaboration will be instrumental in achieving equitable health outcomes and reducing the alarming statistics surrounding Black infant mortality.
Future Directions in Research on Racial Disparities in Healthcare
As research on racial disparities in healthcare evolves, it is imperative that scholars and practitioners continue to explore the complex interplay of factors affecting outcomes such as infant mortality rates. Future studies should delve deeper into the specific causes of healthcare inequality, focusing on access, quality of care, and the structural determinants influencing health outcomes. By shedding light on these critical areas, researchers can provide evidence-based recommendations that inform effective public health policies aimed at bridging the gaps between Black and white Americans.
Furthermore, interdisciplinary approaches involving epidemiologists, sociologists, and public health professionals will enrich the understanding of systemic issues contributing to racial disparities. This collaboration can lead to innovative solutions tailored to meet the needs of marginalized populations. As the focus shifts towards actionable insights derived from comprehensive research, our collective commitment to addressing racism and inequality in healthcare will lay the groundwork for a healthier future, where infant mortality rates are no longer determined by race.
Frequently Asked Questions
What are the current statistics regarding infant mortality rates between Black and white infants?
Recent studies indicate that Black infants face significantly higher mortality rates compared to their white counterparts, currently dying at twice the rate of white infants. This disparity has increased from a 92% higher mortality rate in the 1950s to 115% today, exemplifying ongoing racial disparities in healthcare access and quality.
How do healthcare inequality and infant mortality rates relate to racial disparities in America?
Healthcare inequality directly impacts infant mortality rates, particularly among racial groups. Black infants experience disproportionately higher mortality rates due to systemic issues such as limited access to quality healthcare, which highlights the urgent need to address these racial disparities in healthcare to improve outcomes.
What historical trends have contributed to the widening gap in infant mortality rates between Black and white infants?
From 1950 to 2019, while overall life expectancy for both Black and white Americans has improved, the gap in infant mortality rates has widened. Factors contributing to this trend include socioeconomic disparities, access to healthcare, and differences in medical care quality, which have not significantly improved for Black infants.
What are the main causes of excess infant mortality rates among Black infants?
The leading causes of excess infant mortality among Black infants are related to medical issues, often exacerbated by healthcare inequality. Factors such as inadequate prenatal care, lack of access to healthcare facilities, and insufficient quality of care contribute significantly to these mortality rates.
What can be done to address racial disparities in infant mortality rates?
To effectively address racial disparities in infant mortality rates, policymakers must prioritize equitable healthcare access and quality for all racial groups. This includes increasing funding for maternal and infant health programs, improving healthcare accessibility in underserved communities, and instituting policies that target the specific needs of minority populations.
How has the public perception of healthcare inequality affected the discussion about infant mortality rates?
Public perception often acknowledges improvements in healthcare overall; however, this can obscure the persistent and worsening infant mortality rates among Black infants. It’s vital to recognize these disparities in discussions about healthcare improvements to ensure that policies target and remediate these inequalities.
Why is it important to analyze long-term data when studying infant mortality rates?
Analyzing long-term data, such as the comprehensive study covering 70 years, helps to reveal trends and disparities that might be overlooked in shorter studies. This broader perspective is crucial for understanding systemic issues and making informed policy decisions to address inequities in infant mortality rates.
What role do public health authorities play in improving infant mortality rates among different racial groups?
Public health authorities must take an active role in identifying and mitigating the factors contributing to disparities in infant mortality rates. This includes advocating for policies that ensure equal access to quality healthcare, conducting targeted outreach in communities with high mortality rates, and funding research that investigates the root causes of these disparities.
| Key Point | Details |
|---|---|
| Longer Life Expectancy | Overall mortality rates have improved for both Black and white Americans since the 1950s, with life expectancy rising significantly for both groups. |
| Disparity in Infant Mortality | Despite improvements, Black infants die at twice the rate of white infants, with the racial gap in infant mortality worsening over the decades. |
| 70-Year Study Findings | The study analyzed data from 1950 to 2019, revealing a consistent trend where Black infant mortality rates have not only failed to improve but have actually widened in disparity. |
| Major Causes of Death | Medical conditions during pregnancy and healthcare inequalities contribute significantly to the higher mortality rates of Black infants. |
| Healthcare Inequality | Access to healthcare and the quality of care received varies significantly between races, leading to enduring disparities in infant mortality. |
| Call to Action | There is an urgent need for public health authorities to focus on reducing these disparities and improving access and quality of care for Black Americans. |
Summary
Infant mortality rates present a stark disparity in health outcomes between Black and white Americans, which has not improved in several decades. A study spanning 70 years indicates that while overall mortality rates for adults have narrowed, the gap in infant mortality continues to widen alarmingly, with Black infants experiencing a mortality rate twice that of their white counterparts. This situation underscores the urgent need to address healthcare inequalities and enact policies that will ensure equitable access to quality healthcare for all populations, particularly infants, to prevent unnecessary deaths.