Microglial cells research has emerged as a pivotal area within neuroscience, particularly in understanding the intricacies of the brain’s immune system. These remarkable cells play an essential role in monitoring brain health by identifying and eliminating damaged cells, which is crucial for preventing neurodegenerative diseases like Alzheimer’s disease. Groundbreaking studies led by researchers such as Beth Stevens have unveiled the dual function of microglia, especially their involvement in harmful synaptic pruning that can accelerate Alzheimer’s symptoms. As the scientific community delves deeper into microglial function, the potential for new biomarkers and therapies to combat such conditions has significantly increased. This not only brings hope for more effective treatment options for millions but also redefines our approach to the prevention and management of neurodegenerative disorders in the future.
The exploration of glial cells, particularly microglia, represents an exciting frontier in the field of neurobiology. Often referred to as the first line of defense in the brain, these immune cells are integral to maintaining homeostasis and responding to neurological injuries. Research efforts focusing on these brain-resident immune cells shed light on their significant roles in various conditions, including Alzheimer’s and other neurodegenerative disorders. Scientists like Beth Stevens have provided groundbreaking insights into how the activity of microglia can influence synaptic health and overall cognitive function. By understanding the underlying mechanisms of microglia, researchers are paving the way for innovative therapeutic strategies that could transform treatment approaches for millions affected by cognitive decline.
Understanding the Role of Microglial Cells in Neurodegenerative Diseases
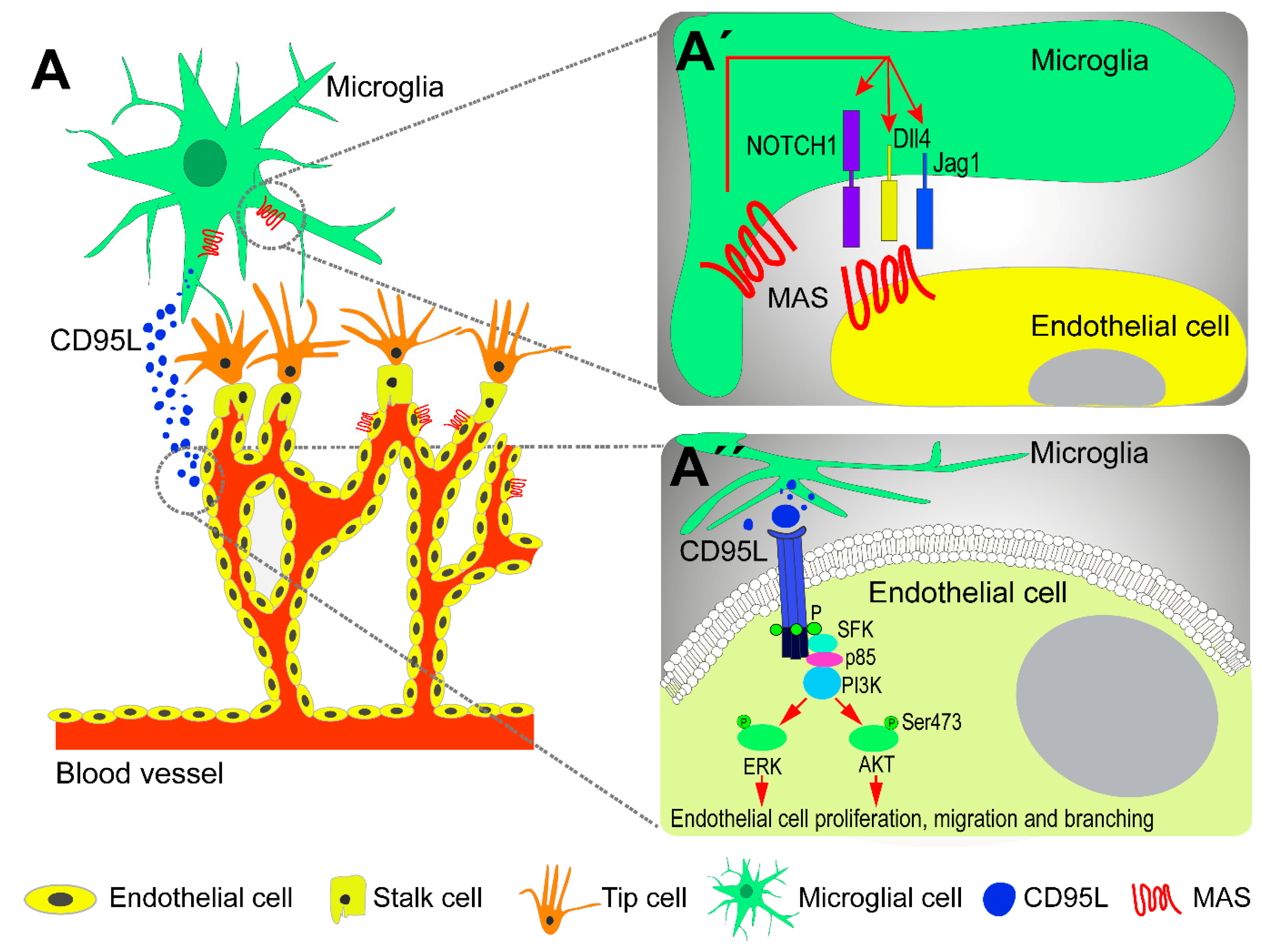
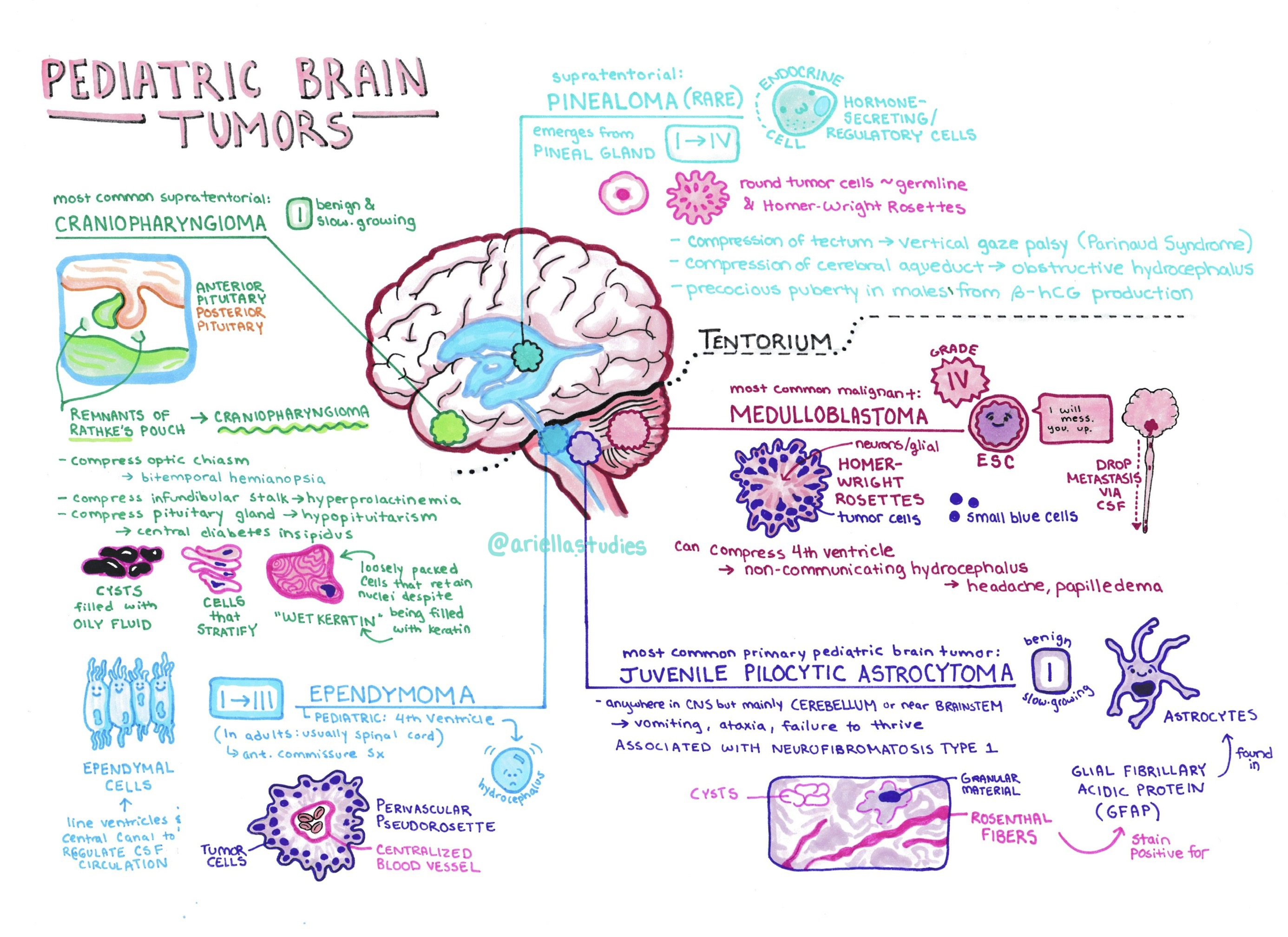
Microglial cells are crucial components of the brain’s immune system, exhibiting a dynamic role in maintaining neural health. These cells continuously survey the brain environment for pathogens and neuronal damage, responding rapidly to any signs of distress. Their ability to clear debris through phagocytosis and to prune synapses during development is well-documented. However, advanced research, especially that conducted by Beth Stevens, has highlighted that an imbalance in microglial function can lead to neurodegenerative diseases such as Alzheimer’s disease. Ineffective pruning of synapses may result in neuroinflammation, contributing to cognitive decline.
Beth Stevens’ pioneering work at the Stevens Lab has brought to light the mechanisms by which microglial cells operate under both healthy and pathological conditions. Not only does understanding microglial cells provide insight into the immune responses of the brain, but it also opens avenues for developing novel therapeutic strategies. By identifying specific markers of microglial dysfunction, researchers hope to create targeted treatments that enhance brain health and prevent the onset or progression of neurodegenerative diseases.
Beth Stevens’ Groundbreaking Research on Alzheimer’s Disease
Dr. Beth Stevens’ research is redefining our understanding of Alzheimer’s disease. Her findings suggest that the malfunction of microglial cells, which are responsible for maintaining synaptic health, can have serious repercussions for cognition and memory. In essence, when these cells incorrectly prune synaptic connections, they can contribute to the early stages of Alzheimer’s disease. This controversial yet innovative perspective indicates that microglia hold the potential key not just to understanding but also to treating neurodegenerative conditions that afflict millions globally.
Stevens emphasizes the importance of curiosity-driven research, stating that her work on microglial function could unlock new biomarkers for early Alzheimer’s detection. Armed with funding primarily from the National Institutes of Health, her lab has diligently mapped out how microglial cells function during both healthy brain development and disease states. This foundational work not only aids in grasping the complexities surrounding Alzheimer’s but also inspires the search for effective treatments that target the underlying mechanisms, rather than just the symptoms.
The Intersection of Basic Science and Clinical Applications
The journey from basic scientific research to clinical application is often long and complex, as illustrated by Stevens’ work. Initially, studies on microglial cells may seem remote from direct health implications, focusing instead on aspects like the visual system in mice. However, as Stevens suggests, these animal models are critical for understanding the human brain’s intricacies. Discovering how microglia respond in specific circumstances provides the groundwork for developing novel treatments for Alzheimer’s and other neurodegenerative diseases.
The significance of federally funded research cannot be overstated in this context. Without initial support, many groundbreaking discoveries, such as those made in Stevens’ lab, would never reach fruition. The interplay between basic research and clinical relevance shows how scientific inquiry can lead to transformative advancements in understanding complex diseases, such as Alzheimer’s. For instance, insights gained through studying microglial behavior could ultimately guide the development of therapies to prevent cognitive decline in the aging population.
The Future of Neurodegenerative Disease Research
As we look to the future, the focus on microglial cells continues to gain momentum in Alzheimer’s research. Innovations in technology are paving the way for more refined studies of microglial behavior in real-time within the brain. This shift allows researchers to observe the interactions of microglia with neurons and understand their role in the progression of neurodegenerative diseases more clearly. Stevens’ ongoing work at the intersection of basic science and clinical application reflects a broader trend in the field toward exploring how immune responses in the brain can be harnessed for therapeutic benefits.
The potential for microglial research to yield new treatments for Alzheimer’s is promising. With better understanding of how these cells regulate synaptic changes and respond to pathology, scientists are hopeful that new approaches can mitigate the effects of neuroinflammation and improve cognitive outcomes for those affected. The ongoing commitment from national funding agencies further underscores the vital role that sustained research support plays in achieving breakthroughs in this challenging field.
Building a Holistic Understanding of the Brain’s Immune System
Beth Stevens highlights the necessity of analyzing the brain as a whole, rather than viewing microglial cells in isolation. This holistic perspective is crucial for understanding neurodegenerative diseases, particularly Alzheimer’s. It is not just about the roles of microglia; it is equally about how these cells interact with neurons and the broader networks within the brain. As researchers gather more data about these interactions, new paradigms will emerge that challenge traditional views of mental health and neurodegenerative disorders.
Moreover, integrating insights from various disciplines such as neuroimmunology and molecular biology will be essential for advancing our understanding of brain health. By emphasizing the interconnectedness of cellular functions, Stevens’ approach facilitates a more comprehensive study of diseases like Alzheimer’s. This multi-faceted strategy may yield innovative pathways for intervention and patient care, driving forward the quest for effective treatments.
Innovations in Biomarkers and Therapeutics
The Stevens Lab has made significant strides in identifying biomarkers associated with microglial dysfunction in Alzheimer’s disease. These biomarkers are crucial for early diagnosis and for monitoring the effectiveness of new therapies. By pinpointing specific genetic and molecular markers, researchers can distinguish between normal aging processes and the pathological changes characteristic of Alzheimer’s disease. Such innovations hold the potential to revolutionize how the medical community approaches early intervention and treatment.
In addition to advancing biomarker studies, the lab is also dedicated to exploring new therapeutics targeting microglial cells. With a better understanding of their role in neurodegeneration, the prospect of designing drugs that can modulate microglial activity presents a tantalizing opportunity for mitigating the effects of Alzheimer’s disease. By focusing on preventing the dysfunction of these immune cells, researchers like Stevens aim to create treatments that address the root causes of neurodegenerative disorders, paving the way for improved outcomes.
The Impact of Curiosity-Driven Research in Neuroscience
Curiosity-driven research is an essential aspect of scientific exploration, especially in complex fields like neuroscience. Stevens’ journey exemplifies how foundational research can lead to unexpected discoveries that reshape our understanding of diseases like Alzheimer’s. By following her curiosity and investigating the functions of microglial cells, she not only advanced her own understanding of neurobiology but also contributed significantly to the field’s collective knowledge about the brain’s immune system.
The value of such an approach lies in its ability to foster innovation and creativity in scientific inquiry. When researchers are encouraged to explore beyond conventional boundaries, new ideas emerge that can lead to breakthroughs in treatment and understanding of various health conditions. Stevens’ work underscores the importance of supporting scientific curiosity through consistent funding and resources, ensuring that vital research into neurodegenerative diseases can continue to flourish.
Challenges and Opportunities in Alzheimer’s Disease Research
Despite the progress made in microglial cells research, significant challenges remain in the field of Alzheimer’s disease. One of the primary hurdles is the complexity of the disease itself, which involves multiple pathways and mechanisms. As Stevens and her colleagues have discovered, microglial cells do not act in isolation; they interact with various other cell types, influencing and being influenced by a multitude of factors. Fully understanding these interactions requires advanced methodologies and long-term studies.
Nonetheless, these challenges also present unique opportunities to further scientific understanding and develop innovative treatments. By leveraging emerging technologies and interdisciplinary collaborations, researchers are equipped to tackle the multifaceted nature of Alzheimer’s. Continued efforts in microglial research not only promise to shed light on disease mechanisms but may also uncover novel therapeutic targets that can be harnessed to address the urgent healthcare challenge posed by neurodegenerative diseases.
The Importance of Funding in Neuroscience Research
Funding plays a critical role in fostering advancements in neuroscience, particularly in niche areas such as microglial cells research. The support provided by national institutions like the NIH allows researchers like Beth Stevens to pursue inquiries that may not initially seem aligned with clinical outcomes. This long-term investment in basic science often yields innovative findings that can transform our understanding of complex diseases like Alzheimer’s.
Moreover, sustained funding is essential for recruiting new talent to the field, enabling the next generation of scientists to explore groundbreaking ideas. As the landscape of neuroscience evolves, prioritizing funding for fundamental research ensures a continuous pipeline of knowledge and innovation. The implications for Alzheimer’s care and treatment are profound, as ongoing research into microglial cells and related factors could lead to effective population-wide strategies for prevention and intervention.
Frequently Asked Questions
How do microglial cells research contribute to our understanding of Alzheimer’s disease?
Microglial cells research, particularly led by scientists like Beth Stevens, has significantly enhanced our understanding of Alzheimer’s disease. These cells act as the brain’s immune system, clearing debris and regulating synaptic pruning. Abnormalities in this process are linked to Alzheimer’s, providing insights into potential biomarkers and treatments for neurodegenerative diseases.
What role do microglia play in neurodegenerative diseases?
Microglia are essential for maintaining brain health and are involved in neurodegenerative diseases like Alzheimer’s. Through their function in pruning synapses, they help shape neural circuits. However, when this pruning process becomes dysfunctional, it can contribute to the progression of neurodegenerative diseases, highlighting the need for ongoing microglial research.
Who is Beth Stevens and what are her contributions to microglial cells research?
Beth Stevens is a renowned neuroscientist whose research focuses on microglial cells and their role in neurodegenerative diseases. Her influential work has uncovered how abnormal microglia function can lead to disorders like Alzheimer’s disease, paving the way for new treatment strategies and a deeper understanding of the brain’s immune system.
Why is studying microglial function important for developing Alzheimer’s disease treatments?
Understanding microglial function is crucial in developing Alzheimer’s disease treatments because these cells directly influence neuroinflammation and synaptic health. Research into their role can lead to identifying new biomarkers and therapeutic targets, ultimately enhancing treatment options for millions affected by neurodegenerative diseases.
What discoveries have been made regarding microglia and their impact on the brain’s immune system?
Recent discoveries in microglial research have shown that these cells not only support the brain’s immune response but also play a key role in synaptic pruning and circuit development. Work by Beth Stevens and others has highlighted how dysregulation in microglial function contributes to the pathology of Alzheimer’s disease and may inform future interventions.
How has NIH funding influenced microglial cells research?
NIH funding has been instrumental in advancing microglial cells research, providing scientists like Beth Stevens with the resources needed to explore innovative questions about brain health and disease. This support has enabled groundbreaking discoveries that are crucial for understanding neurodegenerative diseases, particularly Alzheimer’s.
| Key Aspects | Details |
|---|---|
| Researcher | Beth Stevens, associate professor of neurology at Harvard Medical School. |
| Research Focus | Microglial cells and their role in the brain’s immune response. |
| Importance of Microglia | Clear dead/damaged cells and prune synapses. Their dysfunction can lead to neurodegenerative diseases. |
| Diseases Studied | Alzheimer’s disease, Huntington’s disease, and various other neurodegenerative disorders. |
| Funding Sources | Primarily NIH and federal agency grants. |
| Impact of Research | Potential new biomarkers and treatments for neurodegenerative diseases affecting millions. |
| Quote by Beth Stevens | ‘Our microglial research is a prime example of an immune-related pathway that would never have advanced without foundational research.’ |
Summary
Microglial cells research is paving the way for groundbreaking advancements in understanding neurodegenerative diseases like Alzheimer’s. Through the innovative studies led by researchers like Beth Stevens, we are uncovering the critical roles these cells play in brain health and disease. By combining curiosity-driven exploration with foundational research, scientists are making strides towards identifying new treatments that have the potential to significantly enhance the quality of life for millions affected by such conditions. As the field continues to evolve, the importance of understanding microglial function will only grow in significance.