Pediatric brain cancer represents a particularly challenging area of oncology, impacting thousands of children each year with various types of tumors such as gliomas. Recent advancements in artificial intelligence (AI) have opened new doors for predicting cancer relapse and managing treatment protocols for young patients. Studies indicate that AI tools leveraging temporal learning can significantly enhance the accuracy of brain tumor treatment plans by analyzing a series of brain scans over time. This innovative approach allows researchers to identify children at risk for recurrence more effectively, offering hope for improved outcomes in pediatric cancer management. As we continue to explore the potential of AI in cancer prediction, understanding the nuances of pediatric brain cancer becomes increasingly crucial for evolving treatment strategies and improving patient care.
Childhood brain tumors, particularly malignant gliomas, pose significant challenges for healthcare professionals tasked with providing effective treatment and monitoring for relapse. Terms like pediatric tumors and brain lesions are often used interchangeably but point to the same urgent need for improved predictive measures in oncology. With the integration of AI technologies in medical practices, there’s a burgeoning interest in the use of advanced analytics to forecast cancer recurrence in affected children. By employing methodologies such as temporal learning, we aim to enhance our understanding of tumor behavior and its implications for future treatments. This innovative intersection of technology and healthcare is critical, as it promises to revolutionize how we approach brain cancer management in young patients.
Understanding Pediatric Brain Cancer and Gliomas
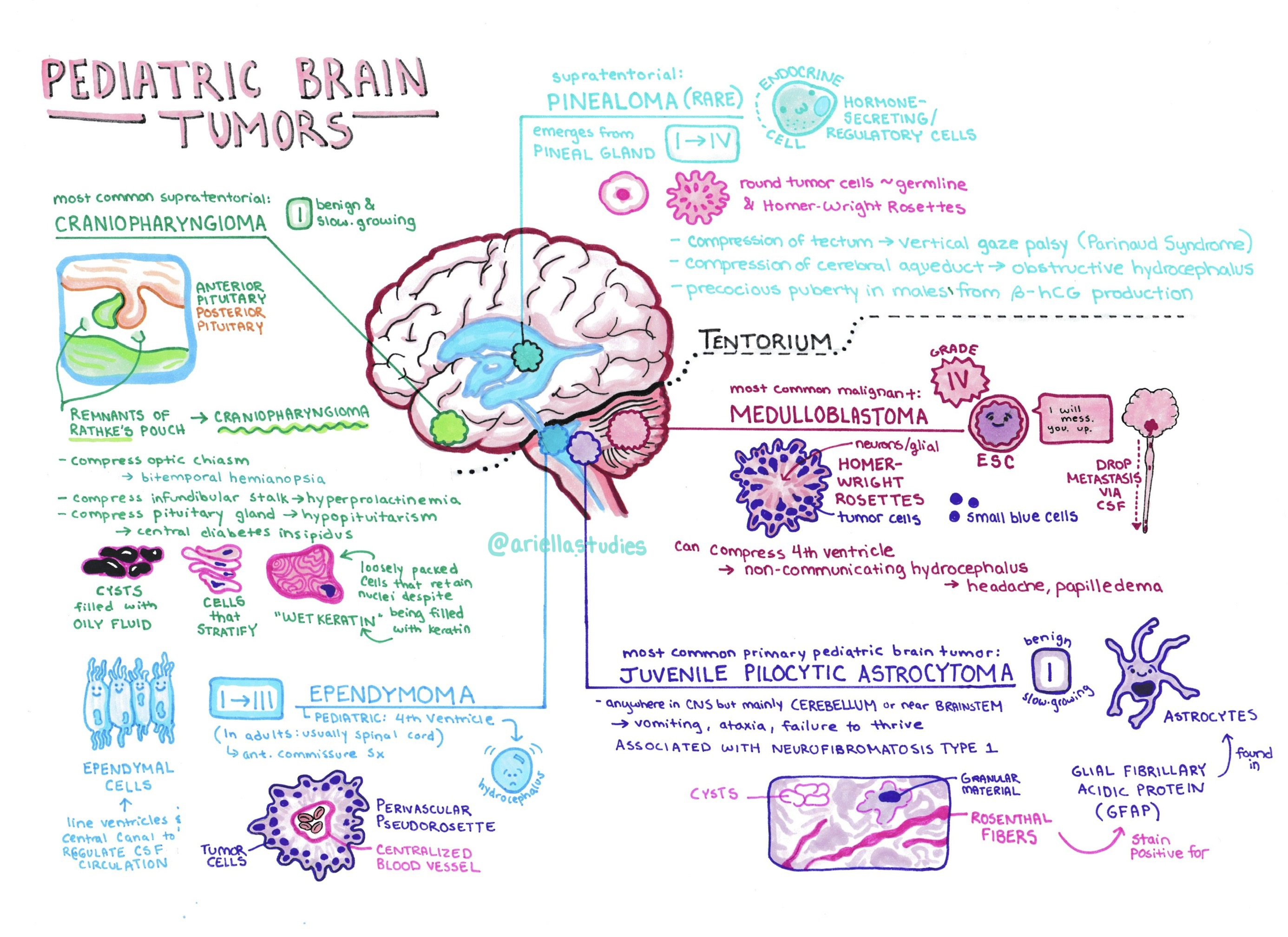
Pediatric brain cancer primarily refers to tumors that occur in the brain or spinal cord of children, with gliomas being one of the most prevalent types. Gliomas can sometimes be benign, but many are malignant and can present severe challenges in treatment and management. Unlike brain tumors in adults, which often relate to lifestyle and age factors, pediatric gliomas are more complex due to the ongoing development of a child’s brain. Understanding the specifics of these tumors can significantly impact treatment protocols, especially when it comes to predicting outcomes like cancer relapse.
The diagnosis and treatment of pediatric brain cancer require a multifaceted approach, as each glioma presents differently based on individual patient factors. This complexity necessitates constant monitoring, particularly after initial treatments. Recent advancements in medical imaging and AI applications are paving the way for better understanding and predicting the progression of these tumors. These tools enable clinicians not only to visualize changes in tumor growth but also to make more informed decisions about interventions, potentially improving the quality of life for children battling these conditions.
The Role of AI in Cancer Prediction for Pediatric Patients
AI technology is revolutionizing how medical professionals predict cancer outcomes, particularly in pediatric cases. In the context of pediatric brain cancer, AI tools trained on historical imaging data can glean insights that a standard analysis might miss. For instance, the study conducted at Mass General Brigham showcases an AI model designed to utilize temporal learning techniques, making it significantly more effective at predicting relapse in pediatric glioma patients than traditional models that often rely on single images captured at isolated time points.
AI can enhance cancer prediction models by integrating diverse data sources, including genetic profiles and real-time imaging, which are critical in understanding the nuances of how gliomas behave over time. With increasing data availability from longitudinal studies, the potential for AI to improve not only immediate treatment strategies but also long-term care plans grows exponentially. As pediatric brain cancer presents unique challenges, incorporating AI into the predictive analytics landscape offers hope for better outcomes through earlier interventions.
Advancements in Glioma Treatment Through AI Techniques
The treatment landscape for pediatric gliomas has evolved significantly with the integration of advanced AI methodologies. By harnessing tools that analyze a series of MRIs over time, researchers have discovered more accurate ways to forecast cancer relapse risk. Such developments mean that clinicians can tailor their approaches more effectively, often predicting the need for additional therapies or simplifying follow-up regimens based on a patient’s specific risk level of recurrence.
Furthermore, the implementation of AI-driven tools encourages a shift towards more personalized medicine in pediatric oncology. By effectively analyzing temporal patterns in tumors, AI can signal when a child may require more aggressive treatment options or when they could safely reduce their frequency of scans, thus alleviating some of the stress associated with prolonged hospital visits. As ongoing studies validate these new models, the prospect for improved long-term outcomes for young patients with gliomas becomes more promising.
Cancer Relapse Prediction: A Game Changer for Pediatric Care
The ability to predict cancer relapse is crucial in the management of pediatric brain tumors, particularly gliomas, where recurrence can significantly impact survival and quality of life. Traditional prediction methods often fall short, giving rise to substantial uncertainty in patient management. The new AI tool developed by researchers from Mass General Brigham stands out due to its use of temporal learning, which allows for a comprehensive review of a patient’s imaging data over time. This capability directly addresses the unpredictability of pediatric cancer relapse, aiming to provide clearer foresight into potential recurrences.
Improving cancer relapse prediction holds transformative potential for pediatric care, offering a pathway to minimize unnecessary treatments and enhance patient monitoring. With accurate predictions, healthcare providers can allocate resources more efficiently, focusing on high-risk individuals who would benefit from more intensive surveillance or treatment options. This paradigm shift not only optimizes clinical outcomes but also reduces the burden on families navigating the complexities of childhood cancer.
Innovative Temporal Learning Techniques in AI Development
Temporal learning, a novel approach in the realm of AI for medical imaging, significantly enhances the ability to analyze sequential data. In the context of pediatric brain cancer, this method examines multiple MRIs over time rather than relying solely on isolated images. Such an approach enables AI algorithms to detect subtle changes that could indicate worsening conditions or impending recurrences of tumors, which is particularly valuable in managing gliomas.
As researchers continue to refine these temporal learning techniques, the implications for pediatric oncology are profound. Not only do they advance our understanding of how brain tumors evolve post-treatment, but they also create opportunities to develop new therapeutic strategies personalized to a child’s specific needs. This innovative use of AI indicates a future where pediatric cancer care becomes increasingly data-driven and tailored to individual patients, potentially leading to better therapeutic outcomes.
Long-term Impacts of AI on Pediatric Oncology
The long-term impacts of AI on pediatric oncology could be revolutionary, particularly in the diagnosis and management of childhood brain cancers such as gliomas. As AI tools become more sophisticated, their integration into clinical practice promises to enhance the accuracy of diagnosis, streamline treatment protocols, and ultimately improve patient outcomes. Ongoing research and collaboration among leading medical institutions are crucial in this endeavor, allowing for the accumulation of vast datasets from pediatric patients.
Moreover, as AI continues to evolve, it could play a pivotal role in fostering a deeper understanding of the biological underpinnings of pediatric cancers. This knowledge could lead to the exploration of novel therapeutic approaches informed by AI insights, which might identify unique characteristics of tumors in young patients that differ from adult cases. Thus, the potential for AI extends beyond immediate treatment—ushering in a new era of oncology that emphasizes prevention, personalized care, and improved quality of life for children diagnosed with cancer.
Collaborative Efforts in Pediatric Cancer Research
Collaboration among research institutions is vital for advancing pediatric cancer research, especially concerning complex cases like gliomas. The study published by Mass General Brigham, in partnership with Boston Children’s Hospital and Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, exemplifies the power of interdisciplinary teamwork. By pooling resources and expertise, these institutions can contribute to a more comprehensive understanding of pediatric brain cancer and develop innovative tools like the AI relapse prediction model.
Such collaborative research efforts can lead to breakthroughs that may not be achievable by individual institutions alone. By sharing data, methodologies, and insights, researchers can accelerate progress in AI applications for cancer prediction, treatment strategies, and ultimately enhance patient care. The continuous exchange of ideas and findings informs future studies, ensuring that advancements benefit the youngest and most vulnerable patients facing the challenges of brain cancer.
Challenges and Considerations in Pediatric Cancer AI Applications
While the potential of AI in predicting pediatric brain cancer relapse is significant, there are challenges and ethical considerations to take into account. Issues such as data privacy, informed consent, and the need for rigorous validation of AI models before implementation in clinical settings are paramount. As pediatric patients are particularly vulnerable, ensuring their safety and well-being during AI applications is essential.
Moreover, the shift towards AI-driven prediction models demands ongoing education and training for healthcare professionals. Clinicians need to understand the limitations and capabilities of AI technologies to make informed decisions about patient care. As the landscape of pediatric oncology evolves, fostering a culture of collaboration between tech developers and medical professionals can ensure that advancements are not only innovative but also ethical and clinically relevant.
Future Directions in Pediatric Brain Cancer Management
The future of pediatric brain cancer management looks promising with the integration of AI technologies and collaborative research efforts. As techniques like temporal learning gain traction, the hope is to develop increasingly precise tools for predicting cancer behavior, thereby shaping treatment decisions and improving patient outcomes. Continued investment in research and infrastructure will be crucial as the field advances.
Looking ahead, one potential direction is the application of AI not just in the prediction of relapse but also in personalized treatment plans tailored to individual genetic and biological markers of pediatric brain tumors. As more is understood about gliomas and their progression patterns, it becomes feasible to integrate advanced AI systems to support decision-making that could one day transform the standard of care for young patients.
Frequently Asked Questions
What is pediatric brain cancer and why is it significant?
Pediatric brain cancer refers to brain tumors that occur in children, with gliomas being a common type among them. These tumors can vary in severity and are crucial to address because they pose significant health risks, including the potential for recurrence, even after successful treatment.
How do AI tools improve the management of pediatric brain cancer?
AI tools enhance the management of pediatric brain cancer by analyzing brain scans over time to predict relapse risk more accurately than traditional methods. This helps in identifying patients at higher risk for tumor recurrence, leading to more personalized and effective treatment plans.
What role do gliomas in children play in the context of brain tumor treatment?
Gliomas in children are a major focus in brain tumor treatment due to their prevalence and varying prognosis. Effective management often involves surgery, but understanding the recurrence risk through advanced methods like AI predictions can significantly improve outcomes and inform treatment decisions.
How does cancer relapse prediction work for pediatric brain cancer patients?
Cancer relapse prediction for pediatric brain cancer involves analyzing multiple MR scans over time using AI techniques like temporal learning. This method allows for a more nuanced understanding of tumor behavior post-treatment, leading to improved predictions about potential recurrences.
What is temporal learning in AI and how does it relate to pediatric brain cancer?
Temporal learning in AI refers to a method that trains models to analyze multiple brain scans taken over time, rather than single images, enhancing the accuracy of predictions regarding recurrence in pediatric brain cancer patients, particularly gliomas.
What are the implications of improved prediction accuracy for gliomas in children?
Improved prediction accuracy for gliomas in children suggests that healthcare providers can better tailor follow-up care, potentially reducing unnecessary imaging for lower-risk patients while ensuring more intensive monitoring and treatment for those at higher risk of cancer relapse.
Why is early identification of relapse risk vital for pediatric brain cancer patients?
Early identification of relapse risk is vital for pediatric brain cancer patients as it allows for timely interventions that can significantly improve their prognosis, reduce the emotional and physical burden on families, and optimize overall treatment strategies.
What advancements are being made in the treatment of pediatric gliomas with AI?
Advancements in the treatment of pediatric gliomas with AI include the development of tools that can predict the likelihood of cancer recurrence with high accuracy, guiding clinical decisions, and potentially leading to proactive treatments and tailored follow-up protocols.
How can AI-informed predictions impact the future of pediatric brain cancer care?
AI-informed predictions can revolutionize pediatric brain cancer care by offering precise tools for monitoring patients, enabling targeted therapies for at-risk individuals, and improving overall treatment strategies to enhance patient outcomes.
What steps are needed before AI can be implemented in clinical settings for pediatric brain cancer?
Before AI can be implemented in clinical settings for pediatric brain cancer, further validation through additional studies and clinical trials is necessary to confirm the effectiveness of AI predictions and their impact on patient care.
| Key Point | Details |
|---|---|
| AI Tool Development | An AI tool was developed to analyze brain scans for predicting recurrence of pediatric brain cancer. |
| Improvement in Prediction Accuracy | The AI achieved a 75% to 89% accuracy in predicting recurrence, improving substantially over the traditional method’s 50% accuracy. |
| Technique Used | The model employs ‘temporal learning’ which assesses multiple scans over time, unlike traditional models that analyze single images. |
| Collaboration and Scale | Conducted by Mass General Brigham in collaboration with Boston Children’s Hospital, using nearly 4,000 scans from 715 patients. |
| Future Implications | There are plans for clinical trials to evaluate if AI-informed predictions can improve patient care. |
Summary
Pediatric brain cancer continues to be a pressing concern, especially for conditions like gliomas. This recent study demonstrates the potential of an AI tool to significantly enhance the prediction of relapse risks in pediatric patients. By employing innovative techniques such as temporal learning, researchers have improved the accuracy of recurrence predictions, which could revolutionize patient management and follow-up care. With ongoing support and further clinical trials, the integration of AI into pediatric oncology could lead to more tailored and effective treatment pathways, ultimately aiming for better outcomes for young patients.